Diabetes-Related Facebook Posts
I wanted to add some of the posts I’ve made on Facebook over the last year.
June 27, 2014
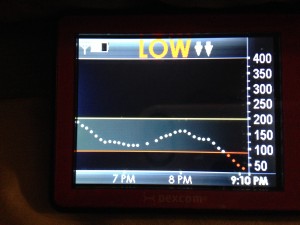
Okay, friends – we need help. We really need a cure for type one diabetes. Lyla is fairly resilient, but I don’t know if I can say the same for myself. Her blood sugar dropped to 29 at 2:30 this morning (normal is around 100). That is the lowest she has ever been. She was mostly asleep, but was very unsettled. I laid in her bed with her and held her, hoping the juice would kick in before she started to seizure. It was terrifying. Last night we went to the Lehi Rodeo. I let her pick out one treat to eat there, and carefully dosed her for it. She was so excited about her treat that she didn’t seem to notice or care that all of her cousins around her were eating lots of snacks and treats. I am tired of having to choose between her physical health and her psychological health (letting her be a “normal” kid). I am tired of her life hanging by a thread. I’m tired of attending every game, practice, class, birthday party and playdate she goes to, because she can’t be left. I’m tired of hyper-vigilant days and frequently interrupted nights. I’m tired of needles and blood and numbers. Mostly, I’m just tired.
It took a long time for me to go back to sleep last night. I thought about how fragile her life is and how badly we need a cure. Obviously, that lead me to thinking about the JDRF walk and how we are gearing up for the walk again this year. It will be our third year walking and fundraising for the JDRF. We do it because we know they are funding the research that will cure this disease, and we want that more than anything else in the world. Lyla loves walk day (she thinks she is the princess of the walk), but it has also been great for Greg and I to feel of your support. We appreciate you walking with us, fundraising with us, and donating to the cause. Your support helps get us through the days when we just don’t think we can do this anymore. We believe in the JDRF. We know they are getting close to a cure. Please help them get there.
April 17, 2014
My baby girl turned five years old today! It was a day filled with fun, friends, family, and princess things (FROZEN!!). Unfortunately, it was also a day filled with blood sugar highs and lows, finger pricks and insulin doses. We went to play at Kangaroo Zoo this morning – her blood sugar was 256 when we got there and 30 minutes later she was at 68. We gave her a juice box, which usually brings her up quickly, but 10 minutes later she was at 52. After another juice box, she finally got up to where she should have been. When her blood sugar was low, she was lying on the chair saying she wanted to go home and didn’t want to jump anymore (so not like her!). I hate that she has to deal with diabetes, especially on holidays and birthdays. We have always supported and advocated for the Juvenile Diabetes Research Foundation (JDRF) because they are funding research that will hopefully cure type one diabetes. Please consider donating $5 to the JDRF in honor of Lyla for her fifth birthday. Hopefully someday she will have diabetes-free birthday!
August 2, 2013
Greg and I had errands to run in Orem and Provo, so we told the kids we would stop at the Disney store if they were good. Lyla sang and skipped the whole way in. I stopped to check her blood sugar once we were in the mall. She was 52 (for reference, 100 is what non-diabetic bodies automatically regulate to) I grabbed skittles from my purse and fed her half a bag and figured that was more than sufficient. We got to the store and within two minutes she was sitting on the floor. Checked her again. 45. TERRIFYING. She had continued to drop even with the skittles. I reached for a juice box in my purse only to realize they were all gone. Greg literally picked her up and ran her to the food court, trying to keep her talking on the way because she looked like she was zoning out. He got her a full sugar soda and she was back to skipping and dancing within 15 minutes. I wish her parents recovered so quickly! It is times like this that remind me why I advocate and fundraise for the JDRF. We really need a cure.
A Day in the Life of a Little Diabetic
In celebration of World Diabetes Day, we wanted to do a day in the life of a little diabetic. World Diabetes Day is focused on raising awareness for both type one and type two diabetes, but obviously our focus is more on type one. Most of you have heard me say this repetitively, but the biggest difference between the types of diabetes is that type one is an autoimmune disease. While the cause is still unknown, it is most likely caused by a combination of genetic factors, influenced by environmental or pathogenic triggers. The immune system is triggered to kill off the islet cells in the pancreas, which make insulin. Without insulin, the cells in the body cannot receive glucose (energy) and the body will slowly die. The only treatment is to inject insulin into the body in appropriate amounts, which is much easier said than done. There are so many factors that influence insulin needs and absorption, making diabetes management very difficult.
Anyway, back to our day . . . Our life is very much the same as any other family with small children. We play, read stories, have tantrums, do chores, fight and laugh. In every way possible, we try to treat Lyla like a normal child and make her feel as normal as possible. From a parenting perspective, diabetes is just one more thing we have to deal with. The closest thing I can liken it to is potty training. When potty training, the parent is required to have a constant vigilance concerning the trainee – when did they last go, how much have they had to drink, do they look like they need to go? Potty training is typically easier when at home, and creates worry and sometimes disaster in other situations. Diabetes is similar, with two major differences; first, it is not a phase that we will pass through quickly and rarely have to deal with again. It is our life and always will be. Secondly, failures in diabetes management are much more severe than any failure I’ve seen while potty training. After all, it can mean death.
Our biggest fear is obviously insulin shock, which can occur if Lyla’s blood sugar goes too low. It is more of a concern at night, as she could slip into a coma and potential die before we ever noticed. While it rarely occurs, type one diabetics can die in their sleep, a fact that haunts us on a daily basis. Greg does the vast majority of nighttime checks, especially now that I am pregnant and tired. Even when I’m not pregnant and tired, he checks most of the time. He’s just awesome like that.
The day technically began at 12:33 a.m., when Greg checked Lyla before he went to bed. He trades off between going to bed early and setting an alarm for 2 or 3 a.m., and going to bed late and checking her before he sleeps. At this middle of the night check, her blood sugar was 215. She is supposed to be between 100-200, and we usually prefer she stay closer to 100. At night, though, we are happy with numbers slightly higher to give her more of a buffer from falling low. Greg decided to let her be at 215 because giving insulin could make her fall too low in the night. It is a constant debate between letting her blood sugar be slightly higher than it should be versus getting up more times of the night. If it were just one night, it would be an easy decision, but it is every night at our house. So we weigh out our sleep needs with her blood sugar numbers. At night she is supposed to be at 175, so 215 is only slightly high. We all need the sleep.
The kids were up at 7:30. I always breathe a sigh of relief when I hear Lyla’s voice in the morning. I worry every single day about her not waking. We check her blood sugar first thing in the morning. She was at 172. Lyla has always had a hard time responding to insulin in the morning. We have struggled with it since diagnosis. It seems to take a long time for her body to respond to the insulin, which usually results in high blood sugar. Typically insulin takes 60-90 minutes to respond in the body, but Lyla takes much longer in the morning and is faster the rest of the day. The only strategy that has slightly helped with this is to give her insulin at least 30 minutes before she starts eating. This is a challenge in the morning because she is usually hungry and wants to eat as soon as she gets up. We allow her to pick a television show to watch to distract her between when the insulin is given and when she can eat. It usually works, though Nick complains horribly about wanting food. In general, we try to apply all rules to both kids, as to not single her out. It works occasionally. Another challenge with administering insulin early is that we have to make an estimate of how many carbohydrates she will eat for breakfast. We generally dose her for 30 carbs, then try to get her to eat accordingly. It does get to be difficult when she wants more food and a food that is higher in carbohydrates. We have also noticed that certain foods break down more easily in her system and keep her more stable. She loves oatmeal squares cereal, for example, but even if we meticulously count carbs and measure portions, her blood sugar is sky high all morning after eating it. On the other hand, Lucky Charms breaks down well. Again a trade-off – healthier breakfast or better blood sugar.
Lyla has an insulin pump, which is like an IV line into the skin, making it easier to give her insulin and give her small amounts. The pump is programmed to the ratios and ranges Lyla should be in, and will calculate how much insulin to give her, making the math portion of diabetes much easier. I enter in that she will eat 30 carbs and it knows what her blood sugar reading was, so it calculates how much insulin she needs. This morning it was 2.45 units of insulin. She watched her television show and then ate breakfast. She wanted orange juice and Lucky Charms. One of the tricks with breakfast is trying to make her breakfast equate to the 30 carbohydrates that we previously dosed her for. We are often a few over or a few under, which can affect her blood sugar later in the morning. One of my least favorite things is telling her no when she asks for seconds or for additional food. Her blood sugar is so bad in the morning, that I hate giving her more to eat because the numbers are so awful, even with additional insulin.
We don’t typically check Lyla’s blood sugar for the first couple of hours after breakfast because she is almost always high. Around mid-morning, the insulin finally seems to kick in and she drops quickly. This is her most unpredictable time of day. Today was a non-teaching day for me, so we had lots to do. We went to story time at the library, then headed to the store. I wanted to make sure she was okay before the store, so we checked after story time. She was at 235. I debated giving her insulin or letting her be. Especially in the morning, it is difficult to determine if the insulin has kicked in or not. If it was still in her system, then I needed to let her be. If it was already through her system, I needed to give her more to bring her down. Because we were heading grocery shopping, I decided to let her be and check her when we got home.
We had several stores to go to and the kids were restless by the time we got to the last one. Nick asked if they could have treats. I normally don’t get them treats at the store, but decided it was warranted because they had been relatively good throughout all the shopping. I let them each pick a small treat. I was thrilled when Lyla chose a sucker that I didn’t think she would like. Then I briefly felt guilty for letting her pick something that she probably wouldn’t eat.
We got home and started unloading groceries. I was busy trying to get everything out of the car and get the perishables put away. Both children were whining. It was nearly lunchtime and they were tired from shopping. I decided to check Lyla’s blood sugar, and she was at 68. Too low. I gave her a juice box while I continued to unload the groceries. When Lyla is low, she gets hungry and wants to eat a lot. As I unloaded the groceries, she spotted the cheese and asked for a piece. That was easy enough, cheese has no carbohydrates. Then she saw the cutie oranges and wanted one. With more carbohydrates being consumed, she needed insulin. I put 10 carbs for the juice and 5 carbs for the cutie into her meter. It took into account her low blood sugar and told me she needed 0.35 units of insulin. I gave her that, so grateful for the meter that does the math and the pump that allows for tiny amounts. Back when we were on shots, she was required to have half unit increments, which was so much harder.
After the cheese and the orange, she wanted an apple and her sucker from the store. I didn’t think she’d like the sucker and wasn’t sure she’d eat the whole apple. I dosed her for another 15 carbohydrates to account for what I thought she would eat of the two, which was another 0.85 units. She ended up eating the whole sucker and half the apple, so I checked her again an hour after eating to make sure she had enough insulin. Sure enough, she was higher than she should have been, at 227. I gave her another 0.45 units of insulin.
At 2:30, I decided to lay down for a minute (this pregnancy is kicking my butt) and wanted to make sure she hadn’t fallen too low before I did. She was at 236. Maybe I should have picked a different day to document? Seriously, not our best, but not completely abnormal either. I have no idea why she wasn’t going down. We rarely have a good explanation for any number. Her blood sugar and insulin needs are constantly changing based on the food she eats, the energy she expends, her excitement levels, and most other emotions. In addition, food can break down more slowly than we expect, or she can have air bubbles in the tubing of her pump, or her pump site can go bad, or the insulin in her pump can go bad. There are so many factors that it is really difficult to pinpoint what is going on.
By 3:10 she wanted a snack, so I dosed her for another 10 carbohydrates. I didn’t check her because I felt I had already checked her more than normal this afternoon. Our insurance will only cover so many test strips a month, so we try to conserve where we can. The strips also retail for over a dollar a piece, so it is very expensive to check her.
At 4 p.m. I was on the phone with the medical supply company to get Lyla’s test strips and pump supplies reordered. I was grabbing a pen from the cupboard, when a very cranky Nick saw the gummy worms in the same cupboard and started screaming for them. Like any mother on the phone, I threw one to him to make him stop screaming so I could hear the lady on the other end of the phone. Of course, then Lyla wanted a gummy worm and started loudly complaining. I gave her one and checked her blood to see where we were at. She was at 150 – in a good range, but definitely too high to have candy without being dosed for it. I dosed her for another four carbs.
We had dinner at 5 p.m. and she was 186. We were having apples, lasagna and garlic bread. We try to dose Lyla before she eats so her blood sugar doesn’t get too crazy high before the insulin kicks in. It is a guessing game to figure out how many carbs she will eat in the meal. Like any other kid, she has days where she eats really well and others where she barely eats anything. I figured 30 carbs was a good starting point since all of the items served were pretty carb heavy.
Of course, she didn’t touch the lasagna and came to me at 6 p.m. saying she was too tired to clean her toy room. This is actually a common complaint for her and we usual have to check her to determine if it is a blood sugar problem or a laziness problem. This time it was legit – blood sugar of 54. I asked what she wanted and she excitedly asked for some of her Halloween candy. She perked up quickly after eating a little candy, but started complaining of not feeling well as soon as I sent her back to finish her chores. Another internal debate – check her again, just in case she is having a crazy plummet, or tell her she is fine and needs to get her chores done. It is hard to figure out when she really doesn’t feel well and when she is trying to get out of something. Both happen a lot at our house. I checked again at 6:30 and she was 132.
Just before bedtime, I needed to change the site for Lyla’s pump. The sites have to be changed every 2-3 days. Lyla’s numbers are better the newer the site is, so we try to change her on Sunday, Tuesday and Thursday evenings so her site will work well at preschool and Grandma’s house while I’m at work. The site change requires a fairly long needle that threads a tube just under her skin. The site should go into fatty tissue, such as the stomach, arms, thighs or a butt cheek. We stick with butt cheek locations because Lyla is so petite that she doesn’t have much fatty tissue elsewhere. Lyla is incredibly tough when it comes to site changes. She made a deal with us a year or so ago, requiring four Swedish fish for a site change. We bribe her with candy – ironic, I know – but she never complains and rarely cries. She is one tough kid. There are times, in fact, when she asks for a site change because she wants candy. Tonight she didn’t want Swedish fish, but wanted a piece of Halloween candy instead. She chose a box of Dots and after she had consumed them, I looked up the carb count and it was way higher than Swedish fish normally are. Not the best choice. Her blood sugar was 134 before the site change. We also have to change out the cartridge full of insulin that goes in her pump and the tubing that goes in her site about once a week. In general, Greg is better at getting the air bubbles out of the cartridge and I am better at getting the sites in without pain. We stick to our strengths, but also switch from time to time so we are both well versed in both tasks.
I checked Lyla’s blood sugar one more time before I went to sleep. Luckily she doesn’t wake when we check her in the night. She was at 128. Greg will check her again when he gets home from work, then he’ll decide on his late night strategy for checking Lyla’s blood: either choosing to have his sleep interrupted at least once, possibly twice or more; or stay up late and only sleep a total of five to six hours, but without interruption. Then we’ll start the process over in the morning.
As overwhelming as it seems, diabetes is only one part of our lives. We have the normal tasks of cleaning, cooking, laundry, grocery shopping and general household management. We also have two small children that need and deserve our time and attention. This is all in addition to two very stressful and demanding careers. Greg is also working on writing his dissertation for his PhD and I am nearly in the third trimester of my worst pregnancy. I certainly do not detail this to complain, but to create awareness. We have lots of friends and family who don’t really understand why we advocate and fundraise for a cure for type one diabetes. To us it is obvious. We want to do everything we can to treat the disease, but we want more than anything for Lyla to be normal and healthy and for her diabetes to be cured. I’m not sure what we would do with ourselves if we didn’t have the constant stress and worry. I’d love to find out.
Diabetes Camp – September 2011
From the time Lyla was diagnosed, we heard about diabetes camp and how amazing it is. For Lyla’s age group, they do a family camp for three days over a weekend. Initially I was going to do it and then started to have second thoughts as the summer progressed and I imagined how difficult it would be to camp with two babies. About a week before the last family camp, we got a postcard in the mail saying we could sign up for Saturday only of the family camp week. Greg and I talked about it and decided it might be a good thing for us to do.
As the day approached, I started to have some serious second-thoughts about it. The camp activities were scheduled from 9 a.m.-9 p.m. and were in Ogden canyon. I started realizing that it would take us nearly two hours to get there and two hours home. The kids would probably be hellions and it would take a tremendous amount of planning. I had everything packed the night before and still was asking Greg if we really should go. The sign up fee was only about $30, so I didn’t feel like we’d be out that much if we decided not to go. Greg kept insisting, so I complied.
The day started early. We were out of the house by about 7 or 7:30. The first directions we had were wrong and it took us much longer to find the campsite than we had planned. We finally got there around 9:30. Immediately an older woman came up to us and tried to take the kids so we could go to the parents class that was being held. Surprisingly, Nick went with her. Lyla had fallen asleep in the car and wasn’t happy. I finally decided we needed to check her blood sugar and suggested that we run to the car and get her kit. The camp volunteers quickly told me they had supplies right there and could check her. They were great with her. The kids were working on crafts and playing on a playground. Lyla would have none of it, so we decided to take her with us to class. She was noisy, though, so Greg went back and did crafts with her. She loved the crafts.
The day was absolutely wonderful. We had several class sessions with parents, had lunch on a beach and were able to play on the beach for a couple of hours, and then the kids had a carnival that night. Even better, we were able to meet other families who have young diabetics. We really saw what a pump looks like and how the parents manage it on young children. All of the teenage volunteers were diabetics and it was good to see so many happy, healthy diabetic children. The kids warmed up to everyone pretty quickly and really enjoyed the time there. It was kind of an odd, but nice, experience for us to allow strangers to watch our children. We so rarely get away anymore, that it was nice to have someone else with them for a while.
Here is Lyla with Amanda, one of the kids’ favorite camp counselors:
A family shot before we left:
We got home after 11. Luckily both kids were asleep before we got out of the canyon. It was a long day, but definitely worthwhile. The next morning, everyone was sleepy and tired:
Six Months Later – August 14, 2011
Breakfast with Rufus – April 16, 2011
The Juvenile Diabetes Research Foundation of Utah has an event every year around Easter time called “Breakfast with Rufus”. Obviously this was our first year to attend the event.
Here are the kids with Rufus, the bear with diabetes:
At the event there was also a very nice vendor fair where Lyla got a new doll and an accessory for Rufus. She chose a little picnic basket for him. We had a good time at the event. I think we’ll be going back again next year!
Honeymooning – March 6, 2011
Lyla has officially hit the honeymoon phase of diabetes. I’m not sure who named this phase. He/she must have a pretty crappy marriage though. For us, honeymooning has not been particularly fun.
Here’s the long and short of it — The islet cells in the pancreas make insulin. For some unknown reason, Lyla’s immune system started fighting off the islet cells. As they started to die, it became harder and harder for the remaining islet cells to regulate her blood sugar. When there were only a few left, they became overworked and under-appreciated so they decided to go on strike. Once the strike began, we started to see the signs and symptoms of diabetes. The few remaining islet cells spent a couple of weeks on vacation (doesn’t that sound nice?!?), having insulin injected to keep blood sugar levels under control. Once they felt rested, they decided to come back to work and contribute to the process. Unfortunately, they aren’t the best workers. They are sporadic and unpredictable.
So, what does this mean for us? It means Lyla’s blood sugars are wild and crazy and we have had almost daily “crashes,” where her body is making insulin and we are injecting it so she goes way too low. The first such crash happened last Saturday. I had gone running with my sister while Greg fed Lyla breakfast and gave her insulin. When I got home, he went ice climbing. Lyla had been pretty good throughout the morning, but her behavior deteriorated fast. She didn’t want to do anything and then she started crying for no apparent reason and wanted to lay on my shoulder. I checked her blood and she was at about 60, which is much too low (ideally she should be 100-200). Truthfully, I just assumed that her blood sugar was low because Greg had miscounted her breakfast carbs and given her too much insulin. It’s not that I don’t trust Greg, but more that I am very comfortable with the nutrition side of diabetes because of my professional training. So, I unfairly attributed it to Greg’s incompetence. I was wrong. I am sorry.
She crashed again on Sunday and twice more on Monday. I talked to the doctor and we slowly started decreasing the insulin we were giving her. On Tuesday morning she was at 270 as I was leaving for work. I gave her a half unit (which is a tiny amount) with breakfast. My mom called less than two hours later to say that she was down to 60 again. I could continue dictating the rest of the week, but really it is more of the same. She has been chronically low and we have been alternating between giving her fruit snacks to get it higher, and giving her less insulin. At this point she hasn’t had any insulin since Friday morning (2 days now). Her body seems to be processing the sugars just fine. It takes a little longer, meaning her blood sugar is high for longer, and she still gets too low sometimes.
Our doctor tells us the honeymoon period can last days, weeks, or months. Everything I have read has warned us that it will end and that she really does have diabetes, even though it doesn’t seem like it right now. In some ways it is really nice not to be counting carbs and giving injections. At the same time, it has made me even more nervous to leave her because she is so variable and her levels have been so wild. So, wildly unpredictable and hugely stressful . . . I’m glad our honeymoon wasn’t like that!
Hospital Adventure – Day Three, February 16, 2011
My morning started by about 7:30 in the hospital. Truthfully, this is actually “sleeping in” for us, since we are usually up by 5 or 6. However, the extreme emotion and sleep deprivation over the last few days made 7:30 feel really early.
I awoke to the resident endocrinologist examining Lyla. I chatted with her for a few minutes. She was actually the only one to ask if we had any family members with endocrine problems. Most of the doctors and nurses had asked if we had diabetes in the family. She asked more broadly, which is interesting because my sister’s boy needs growth hormone shots. We talked about that for a minute. She cited that it was likely unrelated, but still interesting that two cousins would need the same specialists. Dr. Lindsay came in to talk to us again. He seems to be very calm and relaxed. He talked to us about her previous day’s sugar levels and about the modifications he was going to make to our plan going home.
Next, the nurse arrived. Truthfully, she was my least favorite of all the nurses. Yet, I seem to remember her name (Gretchen) while I have totally forgotten the rest (Greg tells me their names were Jessica and Angelina). Anyway, Gretchen made a little list on our white board of everything we needed to do that day. They had originally said we would be there until 5 or 6 that day. Then, the night before they said that we could probably leave around noon. I had considered going home and spending the night at our house with Nick, but figured if we were leaving by noon then the drive was not worth it. As Gretchen was making the list, she speculated that it would be dinnertime before we could leave. We were both disappointed. At this point, Lyla was likely one of the healthiest children in the hospital. We caught the diabetes early enough that she didn’t have ketones in her urine and hadn’t gone into diabetic ketoacidosis. We felt comfortable enough with the sugar testing and insulin shots. In fact, we felt she would do better at home where she would eat normally and nap. Plus, we both badly needed a shower!
Lyla got breakfast and watched the “Price Is Right” while I pumped. Gretchen came in several times while I was pumping and seemed to linger some. It was really quite awkward. During our time in the hospital, when the nurses or staff came in while I was pumping, most of them left quickly. Not Gretchen. She even asked if we wanted to start the education classes, to which I replied that I would like to finish pumping and get my shirt on first.
A different nurse did our education. We talked about hypoglycemia and hyperglycemia. Again, nothing too difficult considering my background. Lyla and Greg colored with her new crayons while we learned. Once the nurse left, we were eager to continue with the teaching so we could get out of there. It turned out that the social worker was not coming. Then the pharmacy reported back that they couldn’t teach us insulin pens on a kid so little. The only things left on the list were more nurse education and the Juvenile Diabetes Research Foundation. They weren’t sure if the JDRF was coming though. We ordered Lyla lunch so it would be there before she got too hungry (sometimes it took up to an hour to get her food). Then Greg decided to take Lyla for a walk so I could start cleaning up and packing the room. I walked out with them for a minute and met Gretchen in the hallway. She informed me that the social worker and pharmacist were not coming and the resident was working on our discharge papers. I was thrilled. She also said, however, that she had sent our medication down to the pharmacy. If we wanted Lyla to eat lunch at the hospital, we’d have to go get the medication. I thought it was pretty flighty of her.
I met up with Greg and Lyla on their walk. Lyla and I continued walking while Greg went into the pharmacy. We got upstairs and saw that Lyla’s lunch was waiting. Greg met us up there a few minutes later. Then we waited for Gretchen for a very long time. We were ready to test Lyla’s blood and let her eat, but at the hospital, they had to check her blood with their monitor as well. Nobody was able to find Gretchen, so we just sat and looked at Lyla’s food. You can imagine how impatient a one-year-old can get when she is hungry and looking at her food.
Finally the tech arrived to do the blood sugar test. We told her that we had struggled to get enough blood for both monitors and had pricked her twice with many readings in order to make it work. We were really hoping to get enough blood so we didn’t have to poke twice. The tech reassured us that we would make it happen. We got Lyla’s finger pricked and the tech put the blood on the strip, only to realize that she had forgotten to scan Lyla’s hospital badge first. We had to do a second poke. Greg was ticked. Lyla was happy just to finally get her lunch and watch Barney. The tech felt so bad that she brought Lyla a necklace and bracelet set, along with some Play-Doh, and found her a new Barney movie to watch.
Lyla slowly ate her lunch. Greg and I were starving, but figured that we could grab something to eat on the way home. Greg even started loading bags into the car. Lyla finished and we were ready for insulin. Again, we struggled to find Gretchen. We waited for quite a while again before we could find Gretchen and give Lyla her shot. We wanted to leave the hospital, but Gretchen said we had one more lesson to do with the educator and needed to do our discharge paperwork. Again, we waited for the educator to become free. Finally she came in and we rushed through the paperwork and lesson. Finally, we were allowed to leave. The tech walked us out to our car to ensure that we were putting Lyla in a carseat.
We left at about 2:30, almost exactly 48 hours after our adventure had begun. Lyla was asleep before we got to Foothill Blvd. We stopped to grab a bite to eat at a drive-thru and then headed home. I was eager to see my baby, but we decided we needed to shower first because Primary Children’s was full of kids with RSV. We got cleaned off and then woke Lyla up. She was not happy to be awake. Finally we went to my parents to get our little baby. He gave us huge grins and was excited to see us. My parents bought us dinner from Cafe Rio and Lyla’s favorite cousin, Ally, came down to visit. Lyla had gotten an old, broken poker from the hospital and pretended to give Ally pokes with it. Nicolas started to fuss, so we finally loaded up to get the kids home and to bed.
We were happy to finally be home with the four of us back together again. Greg started bathing Nicolas. I started to deal with a messy, messy house. We had bags from the hospital, Nick’s bags, and the mess of having chaotically packed. We even had dishes in our sink from Monday afternoon. I began the long process of re-claiming the house when the power went out. The wind outside was horrible as a storm was coming in. I expected the power to return quickly. It did not. I will admit that for the first time during the week, I murmured a little. “Really, God, Are you serious?” I guess He was. So, we sat around with a messy house, trying to decide whether to get the kids in bed in the dark. We finally got Nick down and then got Lyla in her pajamas. She badly needed a bath, but we were worried she’d be cold if the power didn’t come back on and she had wet hair.
I’m sure it was quite the scene to watch Greg and I fumble with the flashlight (we only own one) and try to find Lyla’s supplies to check her blood sugar. As luck would have it, it came back with a value that left us clueless of what to do. It was at 248. Normally, between 200-250, she gets a 1/2 dose of insulin, but those corrections are divided in half at bedtime. Did Dr. Lindsay really want us to give her a 1/4 of a unit of insulin? I know you all cannot see the shot needles, but just trust me that it is a really, really small amount. Further, Lyla is supposed to have a “free” 15 gram carbohydrate snack at bedtime. Was this still the case if her blood sugar was high? We finally called our good friend Laurel, who is an MD, to get some advice (no 1/4 unit, no snack — Dr. Lindsay later told us the same thing. Good job, Laurel!). We gave Lyla a non-carbohydrate snack and as we were finishing, the lights came back on. I was very relieved. I heard the next morning that our neighborhood was the first in Lehi to get lights back and other areas were out until 11 or 1. Maybe God did have some sympathy for me?
I pumped while Greg watched TV and played on his computer. It was the first “normal” moment for us in the week. We were both exhausted and headed to bed fairly early. We set our alarm for 2 a.m. so we could check Lyla’s blood sugar. When she was seven weeks old, we were setting our alarms to get up and feed her so she could gain weight. Here we are again, setting alarms for the middle of the night to attend to her needs. When she asks me why I am tired when she gets older, I will tell her it is because of her.
Hospital Adventure – Day Two, February 15, 2011
Our first full day at the hospital began early, probably around 7, when the nurses and doctors started coming in. Dr. Lindsay was one of the first to come in. I was still laying in the bed next to Lyla (Greg was on the pull-out chair/bed). I don’t remember much of what he and I talked about, but I did ask him if Lyla’s ridiculous amounts of energy had anything to do with her high blood sugar. He laughed and said, “No, if anything she has been more fatigued lately.” I don’t think that is what I wanted to hear!
Once I was up, it took a few minutes to get a menu from the food service people and get Lyla’s breakfast ordered. They had a toddler menu and a carb counting menu, but not a toddler carb counting menu. I guess it just shows how unique she really is. There are not very many toddlers with type one diabetes. She was overly hungry by the time the food came. Her blood sugar was around 80, which is a little bit low. She ate some yogurt, fruit loops, banana, and a bite or two of scrambled eggs. After her meal, the nurses gave her an insulin shot. She did not appreciate it.
We met with the nurse educator after breakfast. As an educator, I was impressed by the structured lessons and teaching. We learned more about diabetes and insulin. Lyla looked at some books and pushed the buttons on the bed while we met. Then a volunteer from the gift shop came up with a balloon and book from Grammy Jackson. Lyla loved the balloon and entertained herself chasing after it for the better part of the morning.
Next we met with the diabetes social worker. I’m not really sure what the point of that visit was. She asked us some questions and talked to Greg about her travels around the world. After she left, we checked Lyla’s blood sugar before she had some lunch. It came back at 450, which is really high. She started eating her spaghettios and peanut butter and jelly sandwiches. She ate and ate. Having had a couple of doses of insulin already, she was starting to get her appetite back. I think she is eating to gain back the weight that she has lost over the last couple of months. Greg ran to get us some lunch while Lyla was eating. I met with the pharmacist to go over all of Lyla’s supplies and medication. Truthfully, it was a bit overwhelming. We have ketone strips that we have to use to test her urine if her blood sugar is too high, a glucagon kit for when her blood sugar goes so low that she passes out, two types of insulin, needles, glucose test strips . . . I’m sure I am forgetting something.
Greg got back from Carl’s Jr about the time Lyla was done eating. Of course, though, Lyla decided she wanted some of our food. This is going to be one of our challenges with Lyla’s diabetes. She asks for bites any time we are eating something. Truthfully, we usually give them to her. She’s gotten to the point where she expects it. Finally, after she had eaten her lunch, and some of ours, it was time to give her another insulin shot. The nurses had been training us in the morning on how to give the shots. We had to give her insulin to compensate for the high blood sugar and to counter the lunch. I know that I got the needle ready. I can’t remember which of us gave her that first shot. I think it was Greg.
After lunch, the hospital dietitian came by to teach us about carb counting. Since I teach nutrition at UVU, a lot of the information was a little too basic. However, this carb counting is totally different from what I am used to. I know calorie counting from when I teach weight management. Carbs are a different beast. It seems a little counter-intuitive for me to not be counting things like butter and fat. The dietitian actually knew several people in the health promotion and education department at the U. We talked about some of the people we knew there. Once the dietitian left, the hospital representative came in to tell us about parent resources at the hospital. We actually didn’t use any of those — except the free continental breakfast, of course.
Lyla should have been taking a nap, but there was no way that girl was going to go to sleep with all the excitement. She really struggles to sleep outside of her crib. I can think of only two times in her life that she has fallen asleep somewhere else in the house. We decided that the nap just wasn’t going to happen, so Greg took her for a walk outside. She was all too happy to be out of her room. She wouldn’t hold Greg’s hand at all, and once they got outside all she wanted to do was run. It was windy out there. Greg had to keep picking her up and putting her back in the grassy areas to keep her from the cars in the busy parking lot, which is of course where she wanted to run. Just being outside made her incredibly happy though. It was actually a really nice day and I lamented that we couldn’t be at home enjoying it at the park. Greg and Lyla were still outside when Tami’s family came to visit. Lyla was so excited to see them, she ran across the parking lot to get to them the instant she saw them, with Greg on her tail, looking for cars and ready to catch the bounding one-year-old should she have fallen. They brought Lyla some stickers, coloring books, crayons and fingerpaints. Plus, they brought her some toys and books from their house. The things from Tami kept Lyla entertained for the remainder of her visit in the hospital.
As soon as Tami’s family left, Lyla crawled up on to Greg and fell asleep. She was totally exhausted after a night of poor sleep, followed by no nap. She had only slept for about five minutes when her dinner came and it was time to check her blood again. This time it was at 50, which is way too low. We tried to get her to eat her dinner, but she completely melted on us. Twice before the diagnosis, we had days where she had done this at lunch. She gets too hungry and then she just starts crying. We try to get her to eat and she refuses. She even spits food out if we try to shove it in her mouth. Usually after much effort, we are able to get something in. Once she starts eating, she shovels food as fast as she possibly can. As she did this in the hospital, we realized that this behavior is a result of low blood sugar. We had thought she was just too hungry, when in fact there was a bigger problem all along. That night at the hospital, we finally got her to eat some fruit snacks, then she was interested in eating dinner. Of course, it helped the we found a Barney video to watch while we ate.
Greg and I decided to take shifts eating in the cafeteria so our little bird would not want bites of our food. Since we are counting every morsel, it is really challenging to let her have bites. Greg went down to the cafeteria and I stayed with Lyla. She ate and watched Barney while I caught up on some work emails.
We gave Lyla her next round of shots just as Greg was returning. A few minutes later, our friend/brother, Dickson came by to visit. Lyla was trying out her new fingerpaints while Dickson was there. She loved them, but was using huge globs of paint. I finally had enough and rinsed her off and let her play with the other toys. I ran down to the cafeteria to get some food at that point. Even though the hospital is decorated so colorfully, it is really quite a depressing place to be. There were a lot of adults in the cafeteria. I don’t think any of them looked well-rested or happy. There is so much sadness in that hospital. I heard the people behind me in line talking about a delayed surgery because of a seizure. It made me really grateful that Lyla “just” has diabetes.
I returned to the room as Greg and Lyla were skyping with Greg and Diana. Then our friend David stopped by with some snacks for us. The nurses also came in to do a bedtime check of Lyla. We got her in her pajamas and ready for bed. I was hoping that because she had slept so little in the hospital, that she would go to sleep quickly and be out all night. I was so wrong. She played around for several hours. At one point, I think it was around 11, I took her for a walk around the hospital. She gained quite a bit of attention from the nurses and staff. Here was this tiny little girl in her pajamas, happily skipping through the halls of the hospital at 11 p.m. She walked down and back up all three flights of stairs. Finally, I decided that I had enough and she was going to sleep. I ended up rocking her for a long time and she finally crashed around midnight. Greg and I stayed up talking for a few minutes about how surreal the whole experience had been. We finally went to sleep at around 12:30. The nurses came in again at 2 to check Lyla’s blood. She cried for a minute and I rocked her back to sleep again. She stayed soundly asleep until probably 8 or 8:30 the next morning. I, unfortunately, did not. The doctors and nurses started coming in at around 7, so I decided it was time to get up then.